Hypercalcemia is defined as a condition in which the serum calcium level is >10.5 mg/dL (the upper limit of normal) or the ionized calcium level exceeds 5.6 mg/dL. The consequences of abnormally high serum calcium can range from asymptomatic to life-threatening. In addition, excessively high serum calcium causes clinical manifestations that affect the neuromuscular, gastrointestinal, renal, skeletal, and cardiovascular systems.1 Malignancy is a common cause of hypercalcemia, particularly when bone metastases exist. Because some tumor cells can resorb or destroy bone tissue, hypercalcemia of malignancy develops more rapidly and more aggressively than hypercalcemia related to other conditions, and includes the classic symptoms of dehydration, anorexia, nausea, vomiting, constipation, confusion, and polyuria. In multiple myeloma, for example, malignant myeloma cells secrete a cytokine-interleukin-6-that activates osteoclasts in the vicinity of the myeloma cells, leading to bone resorption. Hypercalcemia is a common complication of various types of cancer, including squamous-cell carcinoma, multiple myeloma, T-cell lymphoma, and breast carcinoma.
Epidemiology and Etiology
The most common causes of hypercalcemia in the United States are primary hyperparathyroidism and malignancy. Hypercalcemia occurs in approximately 20% to 30% of patients with cancer at some time during the course of their disease, and is encountered predominantly among hospitalized patients, whereas primary hyperparathyroidism accounts for the majority of outpatient cases.1,2
Pathophysiology
There are 4 major types of hypercalcemia associated with cancer, including humoral hypercalcemia of malignancy (HHM), local osteolytic hypercalcemia, calcitriol-secreting lymphoma, and ectopic hyperparathyroidism.2
HHM is the most common mechanism of hypercalcemia in patients with cancer. Many cancer cells secrete parathyroid-hormone-related protein (PTHrP), which binds to the parathyroid receptors in bone and renal tissues, resulting in increased bone resorption and renal tubular reabsorption.3 Local osteolytic hypercalcemia can be differentiated from primary hyperparathyroidism and humoral hypercalcemia of malignancy by normal or slightly elevated phosphate levels, normal levels of immunoreactive PTHrP, and the presence of bone metastases or bone marrow infiltration.
Local osteolytic hypercalcemia is typically associated with breast cancer, multiple myeloma, and lymphoma.1 Moreover, osteoblasts secrete a receptor activator of nuclear factor kappa-B ligand (RANKL), which activates osteoclasts and promotes secretion of insulin-like growth factor-1, which then increases calcium levels, which is a point of target for medications to inhibit RANKL.3
Symptom Overview
Clinical manifestations of hypercalcemia vary according to the level of calcium in the blood. The normal range for total serum calcium is 8.5 mg/dL to 10.5 mg/dL, and the normal range for ionized calcium is 4 mg/dL to 5.6 mg/dL. The severity of hypercalcemia is classified into 3 categories based on the level of total serum calcium (Figure).
Patients with mild hypercalcemia, defined as total serum calcium of 10.5 mg/dL to 12 mg/dL or ionized calcium of 5.6 mg/dL to 8 mg/dL, can be asymptomatic.1 The presenting signs and symptoms of hypercalcemia generally occur when the calcium levels exceed those ranges. Patients whose total serum calcium level is consistently between 12 mg/dL and 14 mg/dL may tolerate this level well, but the sudden development of hypercalcemia in this range or above may lead to dramatic changes in the patient's mental status. The mnemonic "stones, bones, abdominal moans, and psychic groans" represents the constellation of symptoms and signs of hypercalcemia. The clinical manifestations of hypercalcemia can involve many body systems. Central nervous system effects include lethargy, impaired concentration, fatigue, and muscle weakness. Renal effects include dehydration, polyuria, nephrolithiasis resulting from hypercalciuria, nephrogenic diabetic insipidus, and nephrocalcinosis. Gastrointestinal symptoms include nausea, vomiting, anorexia, weight loss, constipation, abdominal pain, pancreatitis, and peptic ulcer disease. Cardiovascular effects include hypertension, shortened QT interval, cardiac arrhythmia, and vascular calcification. Other symptoms include bone pain, arthritis, and osteoporosis.
Treatment Options
This section addresses treatment options for hypercalcemia, including dose, frequency, and titration parameters; expected effects and anticipated time to resolution; special or target populations for specific therapies; and side effects and their management.
The optimal therapy for hypercalcemia of malignancy varies according to the severity of hypercalcemia and the underlying causes. Hypercalcemia related to malignancy may resolve with definitive antitumor therapy directed at the underlying cancer, such as surgery or chemotherapy.3 If it does not resolve with appropriate anticancer treatment, antihypercalcemic therapy focusing on targeting the pathophysiologic mechanisms should be considered. Withholding antihypercalcemic therapy may result in a life-threatening emergency such as coma and death. Asymptomatic patients with mild hypercalcemia (serum calcium level, 10.5-12 mg/dL) generally do not require immediate treatment.
Usual supportive care for hypercalcemia includes removing calcium intake from any sources (eg, intravenous or oral calcium supplements), increasing oral free water intake, discontinuing medications and supplements that cause hypercalcemia (thiazide diuretics, lithium, vitamin D, calcium carbonate therapy), increasing weight-bearing ambulation/activities, and discontinuing sedative drugs and analgesics.1 Symptomatic patients whose serum calcium level exceeds 12 mg/dL or asymptomatic persons whose level exceeds 14 mg/dL should be immediately and aggressively treated with antihypercalcemic therapy: saline rehydration followed by loop diuretics, calcitonin, bisphosphonates, or denosumab.2,4 For the majority of cancer patients with HHM or local osteolytic hypercalcemia, intravenous bisphosphonates or subcutaneous/intramuscular calcitonin or subcutaneous denosumab can be used to inhibit osteoclast-mediated bone resorption.
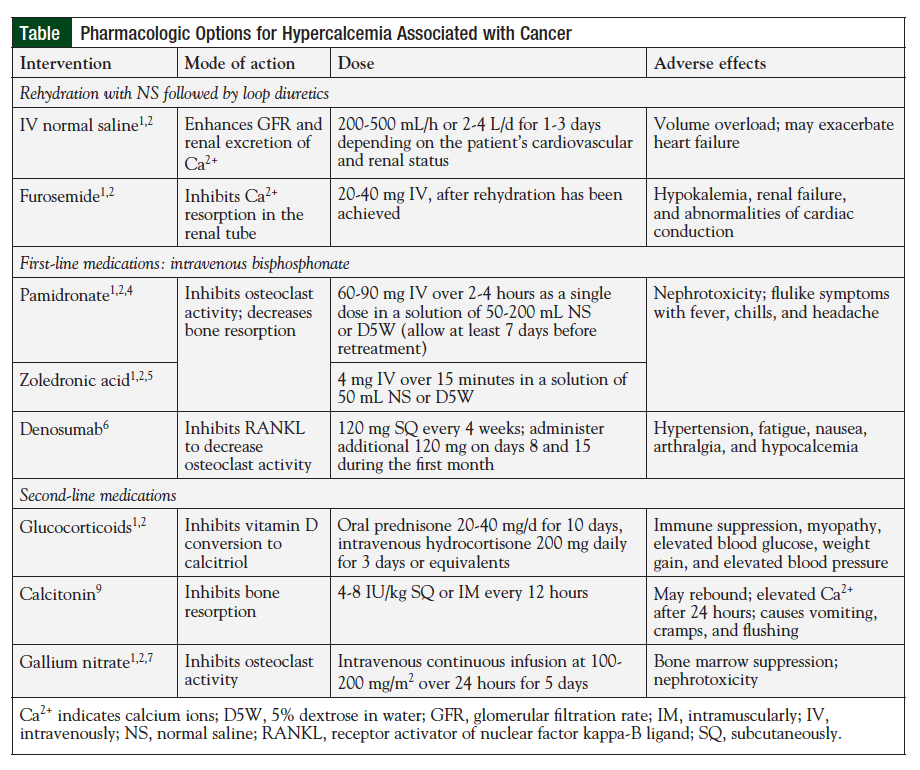
Calcitriol-mediated hypercalcemia is treated with intravenous glucocorticoid therapy plus limitation of calcium intake to inhibit vitamin D conversion to calcitriol.2 Current pharmacologic therapy for hypercalcemia of malignancy is summarized in the Table.
Hydration with Normal Saline Followed by Low-Dose Furosemide
Most patients with hypercalcemia associated with malignancy are dehydrated as a result of renal dysfunction induced by hypercalcemia and by decreased oral fluid intake resulting from nausea and vomiting. Therefore, the cornerstone of initial treatment of hypercalcemia in these patients is volume expansion with intravenous normal saline to increase the glomerular filtration rate and renal calcium excretion.
Rehydration can be accomplished by intravenous administration of normal saline, at a rate of 200 to 500 mL/h or 2 to 4 L/d, depending on renal function, the baseline status of dehydration, and the severity of hypercalcemia. Hydration with normal saline should be continued until the patient is fully resuscitated, serum calcium level is normal, and urine output is maintained at 200 mL/h.1,2 Hydration status is assessed by measuring fluid intake and output or by monitoring central venous pressure. However, aggressive hydration can exacerbate heart failure in elderly patients; thus, the use of hydration is limited in patients with congestive heart failure.
Once intravascular volume has been restored, low-dose furosemide (20-40 mg intravenously) every 1 to 4 hours can be used to further lower the serum calcium level and/or prevent the development of volume overload from administration of normal saline. Furosemide blocks calcium reabsorption in the loop of Henle and increases urine output, which may necessitate increased saline administration, inducing further renal excretion of calcium.1
First-Line Medications
Bisphosphonates
Two bisphosphonate agents were approved by the US Food and Drug Administration for the treatment of hypercalcemia of malignancy: pamidronate (Aredia) and zoledronic acid (Zometa).2-5 Bisphosphonate therapy should be initiated as soon as hypercalcemia is detected, because it takes 2 to 4 days to lower the calcium level. The maximum effect generally occurs within 4 to 7 days after initiation of therapy. In approximately 60% to 90% of patients, the serum calcium level normalizes within 4 to 7 days, and the response lasts for 1 to 3 weeks.2
Bisphosphonates inhibit bone resorption and decrease bone mineralization by disrupting osteoclast activity.2 The most common adverse reactions are renal toxicity, flulike symptoms, injection site reactions, hypocalcemia, hypophosphatemia, fatigue, muscle weakness, and constipation or diarrhea.4,5 Daily oral supplementation with 500 mg of calcium and a multiple vitamin containing 400 IU of vitamin D is recommended to prevent hypocalcemia.4,5
Denosumab (Human Monoclonal Antibody)
Denosumab (Prolia), a full human immunoglobulin G2 monoclonal antibody against RANKL, can be used to manage malignancy-associated hypercalcemia in patients with persistent hypercalcemia despite bisphosphonate treatment. Denosumab binds to RANKL (soluble protein essential for the formation, function, and survival of osteoclasts) and inhibits osteoclast activity, resulting in decreased skeletal-related events and tumor-induced bone destruction.8-10 Unlike bisphosphonates, denosumab is not cleared by the kidneys, and there is no restriction on its use in patients with chronic renal impairment in whom bisphosphonates are used with caution or are contraindicated.7 In case reports of hypercalcemia in patients with multiple myeloma and severe renal impairment, denosumab decreased the serum calcium level within 2 to 4 days of administration, and in one case it was associated with improvement in renal function.7
Second-Line Medications
Glucocorticoids
Glucocorticoids are a treatment option for hypercalcemia in patients with excessive vitamin D or endogenous overproduction of calcitriol secondary to lymphoma.2 In those conditions, agents such as oral prednisone (60 mg/d for 10 days) can be used or intravenous hydrocortisone (200 mg daily for 3 days), or equivalents.1,2
Calcitonin
Calcitonin is an alternative to saline hydration therapy for patients who have severe chronic heart failure or moderate to severe renal dysfunction.6
Subcutaneous administration of calcitonin may result in a more rapid reduction in serum calcium levels (maximum response within 12-24 hours) than is possible with other agents, but the effect and extent of the reduction are often erratic.2
Gallium Nitrate
Gallium nitrate is approved for treatment in hypercalcemia of malignancy. This agent decreases serum calcium by inhibiting osteoclast activity. It is administered by continuous intravenous infusion (100-200 mg/m2 over 24 hours) for 5 days.2 Common adverse events are renal dysfunction, hypocalcemia, hypophosphatemia, decreased serum bicarbonates, and hypotension. Because of the requirement for continuous intravenous infusion, gallium nitrate is not used frequently.2,7
Mithramycin
Mithramycin (plicamycin), a potent cytotoxic antibiotic, reduces serum calcium by inhibiting osteoclast-mediated bone resorption. Mithramycin has been administered via intravenous infusion of 25 µg/kg over 4 to 6 hours in normal saline or a 5% dextrose in water solution.2 This therapy can be repeated daily for 3 to 4 days, and the serum calcium-lowering effect begins within 12 hours of initiation. However, mithramycin is not often recommended for patients with malignancy-related hypercalcemia because of dose-related adverse effects such as nausea, vomiting, stomatitis, thrombocytopenia, renal symptoms, and hepatotoxicity. It is currently not being manufactured in the United States.
Conclusion
Hypercalcemia is a common complication of cancer. Hydration is key, and bisphosphonates are the most popular first-line agents. Denosumab, although expensive, is a valid option for patients with renal impairment. Hypercalcemia of malignancy is a severe complication of cancer that should be treated quickly and appropriately.
Author Disclosure Statement
The authors have no conflicts of interest to report.
References
1. Carroll MF, Schade DS. A practical approach to hypercalcemia. Am Fam Physician. 2003;67:1959-1966.
2. Stewart AF. Hypercalcemia associated with cancer. N Engl J Med. 2005;27:373-379.
3. Hu MI. Hypercalcemia of malignancy: current & future directions. The University of Texas, MD Anderson Cancer Center. Department of Endocrine Neoplasia and Hormonal Disorders Newsletter. 2012;5:1-3.
4. Aredia (pamidronate sodium) [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corp; 2015.
5. Zometa (zoledronic acid) [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corp; 2015.
6. Miacalcic (salcatonin) [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corp; 2015.
7. Lexi-Drugs. Lexicomp. Hudson, OH: Wolters Kluwer Health. 1978-2015. Gallium nitrate; [cited 2015 Aug 21]. http://online.lexi.com.
8. Dietzek A, Connelly K, Cotugno M, et al. Denosumab in hypercalcemia of malignancy: a case series. J Oncol Pharm Pract. 2015;21:143-147.
9. Adhikaree J, Newby Y, Sundar S. Denosumab should be the treatment of choice for bisphosphonate refractory hypercalcaemia of malignancy. BMJ Case Rep. 2014; doi:10.1136/bcr-2013-202861.
10. Prolia (denosumab) [package insert]. Thousand Oaks, CA: Amgen Inc; 2015.